Infertility and cupping
1. Cupping Therapy and
Infertility • Dr Muhammad M El Hennawy • • Ob/gyn Consultant • Rass el barr
central hospital and dumyat specialised hospital • Dumyatt – EGYPT • www.
Mmhennawy.co.nr
2. • If you accept
this lecture, take it as a science • If you not accept it, take it as a fun
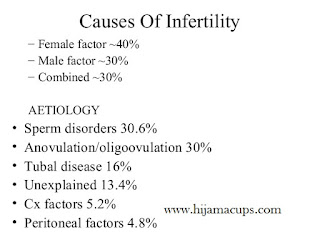
3. Cupping Therapy
• Cupping is an ancient method of causing local congestion. • A partial vacuum
is created in cups placed on the skin either by means of heat (old) or suction
(recent). • This draws up the underlying tissues. • When the cup is left in
place on the skin for a few minutes, blood stasis is formed and localized
healing takes place. • Cupping therapy was originally used in Egypt and China
dating back some 3,500 years • Cupping is applied by acupuncturists to certain
Acupuncture points, • as well as to region of the organ or the area of
dysfunction • as well as to regions of the body that are affected by pain
(where the pain is deeper than the tissues to be pulled)
4. Types of Cupping Therapy • Dry Cupping • Wet Cupping
5. Cupping has also
been found to affect the body up to four inches into the tissues, • causing
tissues to release toxins, • activate the lymphatic system, • clear colon
blockages, • help activate and clear the veins, arteries and capillaries, •
activate the skin, • clear stretch marks • and improve varicose veins. •
Cupping is the best deep tissue massage available. • Cupping, the technique, is
very useful and very safe, being free from side effects and can be easily
learned
6. Infertility • biologically,
inability to procreate can be classified as • Infertility – the inability of a
couple to conceive after one year of unprotected intercourse (6 months for
women over 35) • infecundity (the inability of a couple to produce a live
birth)
7. Causes Of
Infertility – Female factor ~40% – Male factor ~30% – Combined ~30%
AETIOLOGY • Sperm disorders 30.6% • Anovulation/oligoovulation 30% • Tubal
disease 16% • Unexplained 13.4% • Cx factors 5.2% • Peritoneal factors 4.8%
8. Female Infertility
• Female – Ovary – Tube – Corpus – Cervix – Peritoneum
9. Male Infertility
– Sperm count and function – Ejaculate characteristics, immunology – Anatomic
anomalies
(P.T.O)
10. Female Infertility
11. Timing Of
Treatment • around day 5 of the cycle until day 11 (induction-augmentation)
• Ovulation phase (around day 12 of the cycle until day 16)--(triggering
ovulation) • Luteal phase (around day 17 of the cycle until day 28)--(luteal
phase support- improve implantation)
12. Ovulation Disorder stimulate follicle development It is
likely that the hypothalamus-pituitary-ovary axis is involved in cupping
-driven ovulation induction, but the mechanisms involved remain unclear The
result with an average of 38.7% • Hormonal
Infertility
13. For Induction Of Ovulation
(as clomid) • use st28 or st 30 or k13 or Zi Gong or • + or- sp6 • 3 times
in follicular phase • (around day 5 of the cycle until day 11) eg At day 5,7,9
14. For Ovarian
Hyperstimulation for IVF (augmentation of ovulation as hMg( • Bl 23 and Gv
4 • Every 2 day till day of retrieval of ova
15. Some use st28 or
st 30 or k13 or Zi Gong + or- sp6 Plus Bl 23 and Gv 4 In PCOS decrease points
to avoid OHSS
16. Triggering
Ovulation as HCG• Ovulation phase (around day 12 of the cycle until day
16): • Two sessions of Cupping treatment, • using the acupoints CV3, CV4, ST29,
Zi Gong + or - SP6
17. In Vitro
Fertilisation • researchers have remarkably increased pregnancy rates in
women undergoing in vitro fertilisation (IVF). . In the cupping group, 42.5
percent of patients became pregnant, while in the IVF-only group, 26.3% of
patients conceived • Many are using Cupping in conjunction with traditional
medical treatments such as fertility drug • Cupping: Shuidao (ST28), Zhongji
(CV 3) and Guanyuan (CV4) on days 3, 6, 9 • and in some cases 11 • Do with
follicle-stimulating hormone injections • then one prior to having fertilized
embryos transferred into their uterus, • and one directly afterwards
18. PCOS • it
appears that cupping may have a beneficial effect on women with PCOS
(polycystic ovary syndrome) and anovulation, supported by both clinical and
experimental evidence.” • But In PCOS decrease points to avoid OHSS • Start at
morning 8 am for ½ hr
19. Hirsutism •
Add D 14(C7-T1), • St 30 (ovary) • Bl 20(T11) (adrenal)
20. Thyroid
Dysfunction • Add • Si 16 (C3-C4) • D14 (C7) • D12 (T3)
21. Galactorrhea •
Add Gb 34, Gb41
22. Tubal Inflammatory
Block • Cupping is trying in the treatment of female infertility due to
inflammatory obstruction of the fallopian tubes, where it seems to be superior
to conventional therapy with intrauterine injection of gentamicin, chymotrypsin
and dexamethasone • Because cupping stimulates ACTH which increases CORTISONE
which relieves inflammation and edema • Bl32( S2), Cv4 • + or - Bl 20 ( T11)
23. Uterine Cause
• Increase receptivity Of Endometrium-- Cv3 or Cv2 • Decrease contractility of
uterus -- Li 4 • Luteal Phase support –St28, Sp6 or Bl32 • Twice / Week • for 4
Weeks after ovulation
24. Improve
Implantation • “The peripheral impact of cupping in improving uterine
artery blood flow and hence endometrial thickness also provides encouraging
data regarding its potential positive effect on • Cv3 or Cv2
25. Luteal phase
Support • Luteal phase (around day 17 of the cycle until day 28): • One to
two Cupping sessions were given/week. • The acupoints used were ST29, Zi Gong +
or - SP6
26. Endometriosis
• Cv2, Cv4, Sp 8 • + or - D 10 ( T6-T7) + or- Cv 16 • + or – Bl20(T11) • 10
minutes / point/day • Course -- 7 day • Need 2 courses
27. Obesity • Add
D14(C7) • D12(T3) • Bl 10(T6-T7) • Bl 21(T12) • Cv 16
28. Immunological
cause • Add D 10 ( T6-T7) , Cv 16
29. Psycological cause
• Add D20 - D14 (C7)- Bl 19(T6) – D3(L4-L5)
30. Unexplained
Infertility Cv 16 Cv3 or Cv2 St28 or St 30 Si 16 ( C3-C4) D14 (C7) Bl
19(T6) D 10 ( T6-T7) Bl 25 D3(L4-L5)
31. In Clinical
Practice • Cupping physicians typically see about a 30% success rate (depending
on age of patient) to treat infertility. • The treatment course could be
anywhere from 3 to 6 months or up to one year, • depending on severity. • The
outcome can be most rewarding, however. Along with giving birth to a healthy
baby,
32. Observation of the
effectiveness of the treatment for each cause of infertility Cause of
infertility Success rate(%) Ovulatory factor 48% Tubal factor 35% Endometriosis
36% Unexplained 48%
33. Observation of the
effectiveness and the duration of treatment in cases pregnancy Duration of
the treatment Percentage)%( 1st cycle 24% 2nd cycle 25% 3rd cycle 22% 4th –9th
cycle 29% •The results suggest that, among pregnancy cases, about 70% of the
patients became pregnant in the first course (first three months) of the treatment.
•Nevertheless, still close to 30% of the patients became pregnant during the
second or third course of the treatment.
34. How can Cupping help improve my success rate with in-vitro
fertilization? 1. Regulate the hormones to produce a larger number of follicles
2. Improve the function of the ovaries to produce better quality eggs 3. Relax
the patient and decrease stress 4. Increase blood flow to the uterus and
increase the thickness of the uterine lining 5. Strengthen the immune system 6.
Lessen the side effects of drugs used in IVF 7. Prevent the uterus from
contracting 8. Improve semen to create better quality and quantity of embryos
9. Decrease chances of miscarriage
35. Conditions unlikely to respond to cupping - complete blockage of
the fallopian tubes, - extremely low sperm count, - Permanent premature ovarian
failure. In these cases, IVF or other reproductive techniques are usually
suggested
36. Male Infertility
37. Spermatogenesis induction • use C3 + sp6 Plus Bl 23 and Gv 4 •
Every 3 day for 3 month • With good diet • And calm head
38. Thyroid Dysfunction • Add • Si 16 ( C3-C4) • D14(C7) • D12(T3)
39. Varicocele • Add St30 • Bl 21(T12) • Bl 25(L4) – • D 3(L4-L5) •
(S2)28-29 30-31
40. Prostate cause • Add D14 • D12 • Bl 19 • C4 • C2
41. Genital Tract Inflammation • ....” “Males with genital tract
inflammation exhibited the most remarkable improvement in sperm density...” “It
is concluded that cupping may be a useful, nontraumatic treatment for males
with very poor sperm density • ....“A definite increase in sperm count was
detected
42. Sexual Weakness • Add Cv 4-Cv3- Cv 2 • St 30 • D14(C7-T1) •
D12(T3) • Bl 19(T6) • Bl 25(L4) • D3(L4-L5)
43. Obesity • Add D14(C7) • D12(T3) • Bl 19(T6) • Bl 219T12) • Cv 16
44. Immunological cause • Add D 10 ( T6-T7) , Cv 16
45. Psychological cause • Add D20 • D14 (C7) • Bl 19(T6) • D3(L4-L5)
46. Unexplained Infertility Cv 16 Cv3 or Cv2 St28 or St 30 Si 16 (
C3-C4) D14 (C7) Bl 19(T6) D 10 ( T6-T7) Bl 25 D3(L4-L5)
******************************************************************************
NOTE: If you want receive latest update for cupping
therapy (HIJAMA) treatment. Article, Video monthly Sunnah Date and Latest
Hijama Images on your mobile, just add our mobile number + 91 9860515918 in
your contact list and send following details (Name, Address,) in message from
your Whatsapp.
http://www.whatsapp.com/download/