SUBDURAL HEMATOMA
One of the best way to treat such a condition is by way of
Hijamah.
Hijamah is both a gift and a blessing to mankind.
We should NEVER undermine the capability and capacity of the
prophetic medicine- SubhaanALLAH.
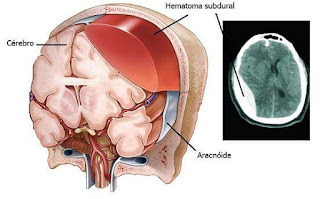
A subdural hematoma is a collection of blood outside the
brain. Subdural hematomas are usually caused by severe head injuries. The
bleeding and increased pressure on the brain from a subdural hematoma can be
life-threatening. Some subdural hematomas stop and resolve spontaneously;
others require surgical drainage.
What Is a Subdural Hematoma?
In a subdural hematoma, blood collects between the layers of
tissue that surround the brain. The outermost layer is called the dura. In a
subdural hematoma, bleeding occurs between the dura and the next layer, the
arachnoid.
The bleeding in a subdural hematoma is under the skull and
outside the brain, not in the brain itself. As blood accumulates, however,
pressure on the brain increases. The pressure on the brain causes a subdural
hematoma's symptoms. If pressure inside the skull rises to very high level, a
subdural hematoma can lead to unconsciousness and death.
Causes of Subdural Hematoma
Subdural hematoma is usually caused by a head injury, such
as from a fall, motor vehicle collision, or an assault. The sudden blow to the
head tears blood vessels that run along the surface of the brain. This is
referred to as an acute subdural hematoma.
People with a bleeding disorder and people who take blood
thinners are more likely to develop a subdural hematoma. A relatively minor
head injury can cause subdural hematoma in people with a bleeding tendency.
In a chronic subdural hematoma, small veins on the outer
surface of the brain may tear, causing bleeding in the subdural space. Symptoms
may not be apparent for several days or weeks. Elderly people are at higher
risk for chronic subdural hematoma because brain shrinkage causes these tiny
veins to be more stretched and more vulnerable to tearing.
Symptoms of Subdural Hematoma
Symptoms of subdural hematoma depend mostly on the rate of
bleeding:
In head injuries with sudden, severe bleeding causing a
subdural hematoma, a person may lose consciousness and become comatose
immediately.
A person may appear normal for days after a head injury, but
slowly become confused and then unconscious several days later. This results
from a slower rate of bleeding, causing a slowly enlarging subdural hematoma.
In very slow-growing subdural hematomas, there may be no
noticeable symptoms for more than two weeks after the bleeding starts.
Symptoms of subdural hematoma can include:
Headache
Confusion
Change in behavior
Dizziness
Nausea and vomiting
Lethargy or excessive drowsiness
Weakness
Apathy
Seizures
People may vary widely in their symptoms of subdural
hematoma. Besides the size of the subdural hematoma, a person's age and other
medical conditions can affect the response to having a subdural hematoma.
Diagnosis of Subdural Hematoma
People who come to medical attention after a head injury
often undergo head imaging, usually with computed tomography (CT scan) or
magnetic resonance imaging (MRI scan). These tests create images of the
interior of the skull, usually detecting any subdural hematoma present. MRI is
slightly superior to CT in detecting subdural hematoma, but CT is faster and
more readily available.
Rarely, angiography may be used to diagnose subdural
hematoma. During angiography (angiogram), a catheter is inserted through an
artery in the groin and threaded into the arteries of he neck and brain.
Special dye is then injected, and an X-ray screen shows blood flow through the
arteries and veins.
Treatment of Subdural Hematoma
Treatment of subdural hematomas depends on their severity.
Treatment can range from watchful waiting to brain surgery.
In small subdural hematomas with mild symptoms, doctors may
recommend no specific treatment other than observation. Repeated head imaging
tests are often performed to monitor whether the subdural hematoma is
improving.
Hijamah for Mild to moderate Hematomas
It is a collection of blood between the cerebral membrane
and the skull
It can very easily be exhumed via the blood vessels that
directly supply nourishment to the organ.
Hijamah not only releases locked blood but also opens up the
lymphatic channels.
So excess fluids can
be drained off naturally into the lymphatic system and the occluded lymph
nodes.
More severe or dangerous subdural hematomas require surgery
to reduce the pressure on the brain. Surgeons can use various techniques to
treat subdural hematomas:
Burr hole trephination. A hole is drilled in the skull over
the area of the subdural hematoma, and the blood is suctioned out through the
hole.
Craniotomy. A larger section of the skull is removed, to
allow better access to the subdural hematoma and reduce pressure. The removed
skull is replaced shortly after the procedure.
Craniectomy. A section of the skull is removed for an
extended period of time, to allow the injured brain to expand and swell without
permanent damage. Craniectomy is not often used to treat subdural hematoma.
People with severe subdural hematomas are often seriously
ill, requiring machine-supported breathing and other forms of life support.
If a person has a bleeding problem or is taking blood
thinners, measures should be taken to improve blood clotting. This may include
giving medicines or blood products, and reversal of any blood thinners, when
possible. Other medications to help reduce swelling or pressure in the brain or
control seizures may also be used.

No comments:
Post a Comment